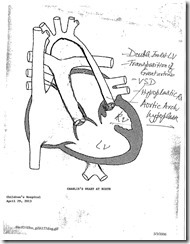
I’ve tried to figure out how to type this post all day. The short version is that surgery was a success yesterday. Charlie spent about 9 hours out of his room from start to finish and tolerated going on and off heart bypass without much trouble. The doctor was even able to close the skin over his open sternum which minimizes the risk of infection (and keeps mom and dad from having to literally watch his beating heart through his chest cavity).
Ultimately, I’ve decided the best way to share Charlie’s story is to share our FaceBook posts from the day. So here they are….
Post #1
So many hearts are breaking now as they start the process to repair one. The anesthetist took Charlie back to the OR to prep for surgery.
Charlie is a strong, tough baby and will get through just fine. It is the time between then and now that is painful for us all.
Post #2
Just received welcomed but scary news: Charlie is successfully on heart and lung bypass and the surgeons have started to dissect his heart.
"Dissect his heart": Those are words I never thought I'd type outside of biology class in high school. Now I type them in reference to my own child with the faith that we'll be able to type them at least two more times in the future.
Right now all is well in Charlie's world, yet it feels like our world is being turned upside down.
Post #3
2:15 update... Just over 4 hours since leaving his NICU room, Charlie remains stable on both heart and lung bypass. His heart has been dissected and they are still in the process of using a graft to enlarge his aorta. This is the longest and most critical part of the surgery. The medical team was hopeful that they would complete this within the next hour and begin warming the room in preparation for eventually taking our little man off bypass.
Please continue to pray for God to steady the hands of the surgeon and for Charlie's heart and lungs to tolerate coming off bypass and working on their own again.
Post #4
3:15 update - 5 hours in they have completed Charlie's repair! They have basically rerouted his entire bloodstream out of his heart and are now double checking everything with an echo. Assuming Dr. Huddleston is happy with his work, they'll begin the meds necessary to wean him off heart/lung bypass.
We're now in a waiting game to see how much blood "leaks and oozes" around his stitches and how Charlie tolerates regaining control of his heart and lungs. This is a big step! Dr. Huddleston told us weeks ago that this would be Charlie's first big test post-op.
Pray that our little fighter passes this first hurdle with flying colors!
Post #5
4:15 update - I'm happy to report that we just met with Dr. Huddleston and Charlie's surgery is officially complete. Charlie handled coming off bypass like a champ! He'll remain on a ventilator until his breast bone is closed up with a second operation (hopefully Friday).
The next 24 hours are critical. It's complicated to explain, but the gist of it is that over the past several months in utero and the last 6 days in the NICU, Charlie's body has learned to function with a malfunctioning heart. Now he has to learn to pump a heart that has entirely different plumbing.
There is still a long road ahead - but we've officially survived the first part of the journey.
Thank you for your prayers over the past few months, today, and in the months to come!
Post #6
Vitals are promising. Oxygen saturation is at 75% and the ventilator was reduced to 80% oxygen mixture. Heart rate and blood pressure are normal.
Celebrate the small victories. He is not conscious and still oozing from the incision. It appears Charlie's body is recovering well. Two hours complete of the critical 24 hours. The marathon has begun and we are pacing with the pack.
Go Charlie!!! YEA!!!!
Post #7
So what does recovery look like?
11 IV solutions
9 sensors with 13 electrodes measuring
3 lines draining fluids
Ventilator ...
As an adult, when you start to run; first your heart beat gets stronger and then you heart rate increases. Because an infant heart does not have the size and muscle development, the only option Charlie has is to increase his heart rate. Along this marathon he is running, his heart rate is normal for an infant without a heart condition. The oxygen has been lowered to 60% and the saturation in the blood remains at 70%.
Charlie has the biggest heart. It may be due to the swelling after surgery, but it is his way of saying, "Thank you for cheering me on." Unlike a real marathon, this trek gets easier as you approach the finish. Keep running Charlie!!!!