Round 2 of explaining Charlie's Cherished Heart
Today I'm only going to tackle one of Charlie's defects:
TRANSPOSITION OF THE GREAT ARTERIES (TGA)
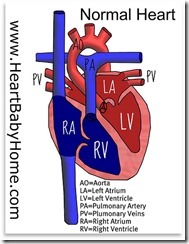
TGA occurs when the two main arteries going out of the heart—the pulmonary artery and the aorta—are switched in position, or “transposed”.
Normally, blood returning to the heart from the body is pumped out of the heart to the lungs. There, it receives oxygen and returns to the heart where it is pumped back out to the body. In other words, blood in a normal heart follows this patterned route repeatedly: heart, body, heart, lungs, heart, body, heart, lungs....
In TGA, blood returning from the body is pumped back out to the body and blood returning from the lungs is pumped back to the lungs. This occurs because the main connections are reversed. Basically, the heart has two closed loops of blood flow. The result of transposition of these two vessels is that too little oxygen is in the blood that is pumped from the heart to the rest of the body because that loop of blood never goes to the lungs to pick up oxygen.
This means that TGA is a cyanotic (lacking oxygen) heart defect that leads to a bluish-purple coloring of the skin and shortness of breath. How bad the symptoms are depends on whether there is a way for the two separate blood circuits to mix, allowing some oxygen-rich blood to get out to the body. This mixing can occur through other defects, such as a hole between the bottom chambers of the heart (VSD), or through a shunt (ductus arteriosus) that normally is present at birth. Luckily (?), Charlie had both of these which is why he was remarkably pink at birth!
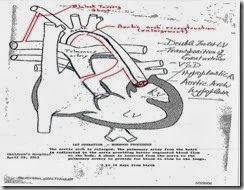
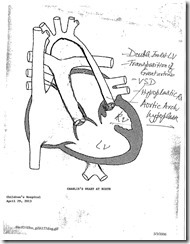
Also, because Charlie has a Double Inlet Left Ventricle all the blood coming back to Charlie's heart (oxygen-rich blood and oxygen-poor blood) is pumping into one ventricle and mixing together creating "partially oxygenated" blood. Then his left ventricle is pumping blood back to the lungs. Charlie's right ventricle is severely underdeveloped (HRHS) causing it to malfunction. Thus, the chamber that should be pumping oxygen rich blood to the body isn't doing it's job and Charlie has poor oxygen saturations compared with the general public.
After Charlie's birth, we relied on that ductus arteriosus mentioned above to keep some oxygenated blood circulating through his little body. This required him to be on special medications to keep that passageway open (it normally seals itself off shortly after delivery).
TGA may be the most confusing part of this whole diagnosis - if you managed to follow this post....tomorrow will be a breeze!